Biopsychosocial Assessment: Why It Matters in Treatment Planning
Question on this topic? Get an instant answer from August.
Here is the blog post you requested.
Biopsychosocial Assessment: Why It Matters in Treatment Planning
What is a Biopsychosocial Assessment?
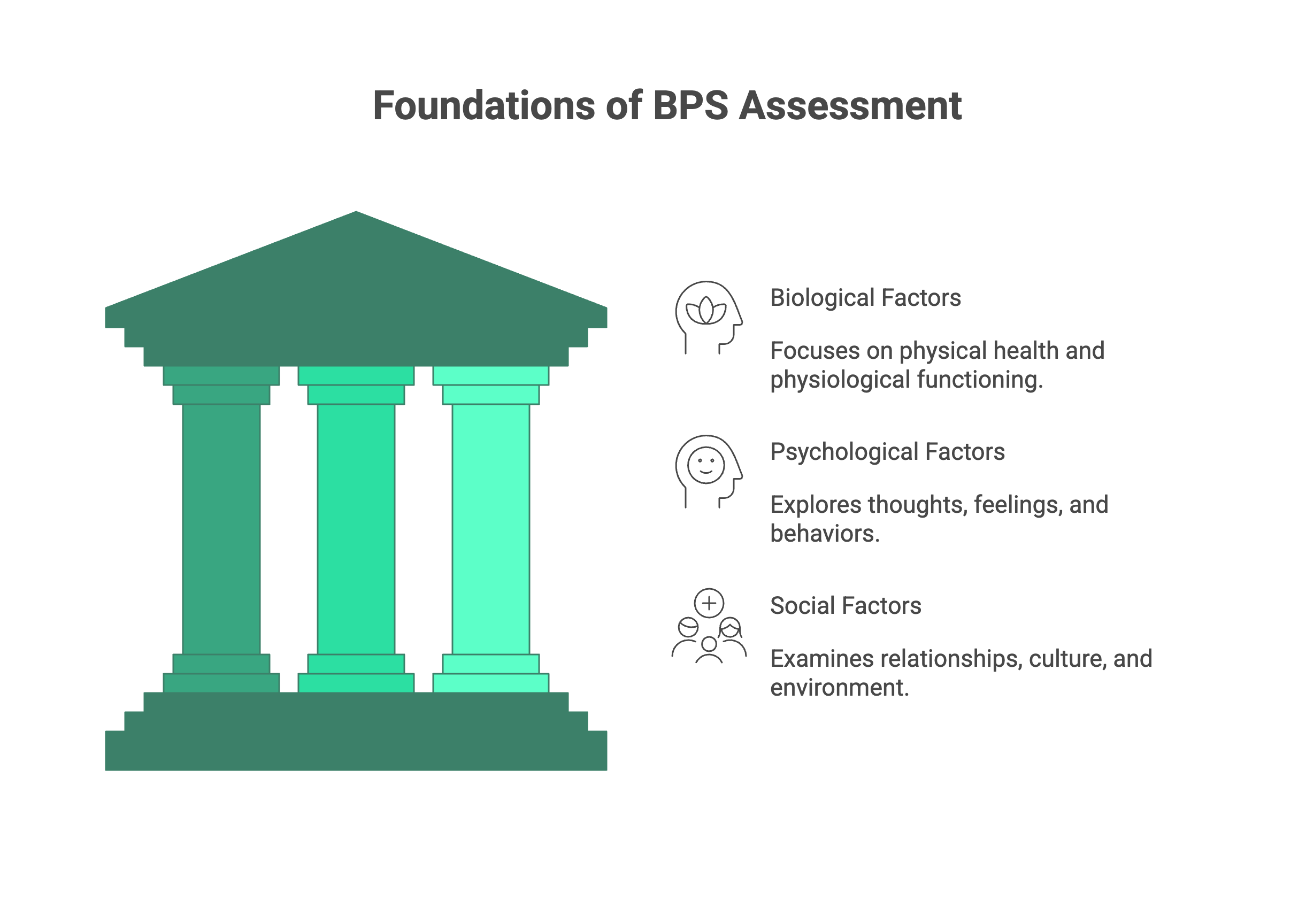
A biopsychosocial assessment, often called a BPS assessment, is a comprehensive evaluation that gathers information about a client’s life through three distinct but interconnected lenses: biological, psychological, and social. Its purpose is to move beyond a simple list of symptoms and create a “whole person” understanding of a client’s challenges, strengths, and context.
Think of it as the backbone of the client’s chart. While other forms of mental health documentation like progress notes track session by session changes, the BPS assessment is the comprehensive map created at the outset of the therapeutic journey.
This approach is rooted in the groundbreaking biopsychosocial model, developed by psychiatrist Dr. George Engel in 1977 source. Engel argued that the prevailing biomedical model which viewed illness as purely a result of physical and chemical processes—was too narrow. He proposed that to truly understand and treat a person, we must consider the dynamic interplay between their body (biology), their mind (psychology), and their world (social environment). This model revolutionized medicine and mental health, cementing the BPS assessment as a cornerstone of effective practice.
The 3 Core Components of a BPS Assessment
The power of the BPS assessment lies in its three pillar structure. By systematically exploring each domain, you ensure no stone is left unturned. Let’s break down these biological psychological social factors.
1. Biological Factors (The Body)
This component looks at the client’s physical health and physiological functioning. The mind and body are not separate entities; their connection is profound. What happens in the body affects the mind, and vice versa.
This area includes: * Medical History: Current and past medical conditions (e.g., thyroid issues, chronic pain, diabetes), surgeries, and significant family medical history. * Medications: All prescribed and over the counter medications, supplements, and adherence patterns. * Substance Use: History and current use of alcohol, nicotine, caffeine, and illicit substances. * Neurodevelopmental History: Any history of developmental delays, learning disabilities, or conditions like ADHD or Autism Spectrum Disorder. * Physiological Basics: Sleep patterns (quality and quantity), diet and nutrition, and level of physical activity. There is a strong link between gut health and mental well being, often called the “gut brain axis” source.
2. Psychological Factors (The Mind)
This is often the most familiar territory for mental health clinicians. It involves exploring the client’s internal world their thoughts, feelings, behaviors, and history.
This area includes: * Presenting Problem: The client’s own words on why they are seeking therapy now. * Mental Health History: Previous diagnoses, past therapy experiences (what worked and what didn’t), and psychiatric hospitalizations. * Current Symptoms: Detailed exploration of symptoms related to mood (depression, anxiety, anger), thought patterns (rumination, obsessions), and behavior (avoidance, compulsions). * Risk Assessment: Thorough evaluation of suicidal or homicidal ideation, intent, and plan, as well as self-harm behaviors. * Coping Skills: How the client currently manages stress, difficult emotions, and challenges. * Cognitive Functioning: General assessment of memory, concentration, and orientation. * Trauma History: Exposure to any form of trauma (abuse, neglect, combat, etc.), including the nature and timing of the events.
3. Social Factors (The Environment)
No one exists in a vacuum. This component examines the external world a client inhabits, including their relationships, culture, and socioeconomic environment. These factors can be powerful sources of both stress and support.
This area includes: * Family and Relationships: Family of origin dynamics, current family structure, and the quality of relationships with partners, children, and friends. * Social Support System: Who the client turns to for support; feelings of connection or isolation. * Education and Employment: Educational background, work history, job satisfaction, and any workplace stressors. * Socioeconomic Status: Financial stability, housing situation, and access to resources. * Legal History: Any current or past involvement with the legal system. * Cultural and Spiritual Factors: The client’s cultural background, identity, spiritual or religious beliefs, and how these factors influence their worldview and well being.
Key Questions to Ask: A Practical Guide for Each Component
Knowing what to ask is half the battle. Here are some sample questions to guide your information gathering for each of the three pillars.
Biological Assessment Questions
- “Could you tell me about your overall physical health?”
- “Are you currently taking any prescribed medications or over the counter supplements?”
- “Does anyone in your family have a history of significant medical or mental health conditions?”
- “How would you describe your sleep patterns? On average, how many hours of sleep do you get per night?”
- “Tell me about your eating habits on a typical day.”
- “How often do you engage in physical activity?”
- “Can you describe your history with alcohol, tobacco, or other substances?”
Psychological Assessment Questions
- “In your own words, what brings you to therapy at this time?”
- “When did you first start noticing these symptoms?”
- “Have you been diagnosed with a mental health condition or received therapy in the past? If so, what was that experience like for you?”
- “When you’re feeling overwhelmed, what do you typically do to cope?”
- “Have you ever had thoughts that life wasn’t worth living, or thoughts of harming yourself or others?” (Follow up with a full risk assessment if indicated).
- “Is there any history of trauma, abuse, or neglect that you feel comfortable sharing today?”
- “What are some of your personal strengths or things you are proud of?”
Social Assessment Questions
- “Who are the most important people in your life right now?”
- “Who makes up your support system? Who do you turn to when you’re struggling?”
- “Can you tell me about your family growing up?”
- “How would you describe your current living situation?”
- “Are you currently employed or in school? What is that experience like for you?”
- “Are there any financial stressors impacting you right now?”
- “Do you have any spiritual or religious beliefs that are important to you or that serve as a source of strength?”
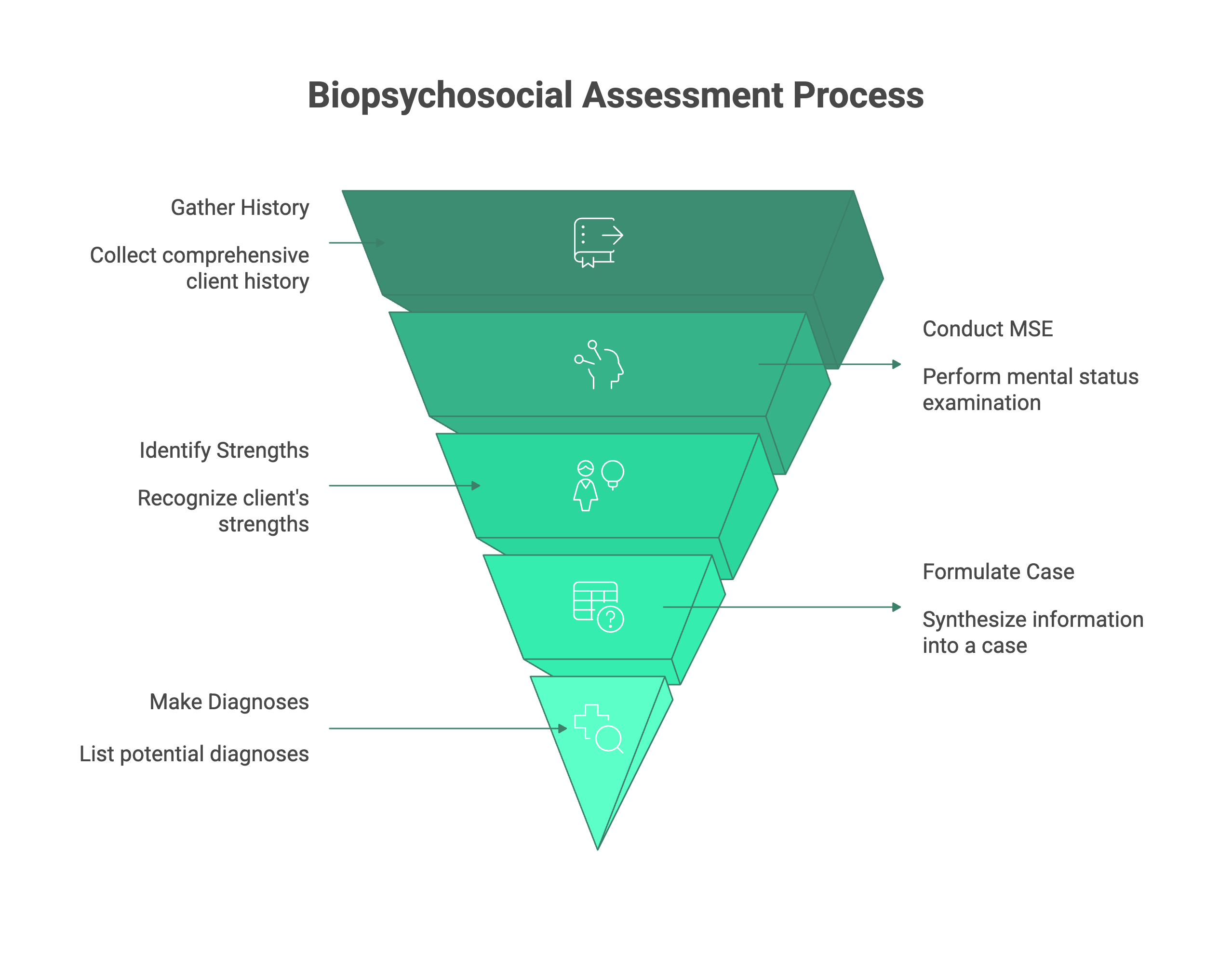
Structuring Your Assessment: The 5 Ps of Case Formulation
Once you’ve gathered all this rich information, how do you make sense of it? This is where a biopsychosocial case formulation comes in. It’s the process of synthesizing the data into a coherent story that explains your client’s situation.
A powerful framework for this is the 5 Ps of biopsychosocial model:
- Presenting Problem: What is the client’s primary complaint? Why are they seeking help now? (e.g., “Client reports experiencing panic attacks three times per week.”)
- Predisposing Factors: What are the historical or background factors that made the client vulnerable to this problem? (e.g., “Family history of anxiety; history of childhood emotional neglect.”)
- Precipitating Factors: What were the recent triggers or events that led to the onset of the presenting problem? (e.g., “Client was recently laid off from their job.”)
- Perpetuating Factors: What factors are maintaining the problem and keeping it going? (e.g., “Client avoids social situations, which reinforces their anxiety; poor sleep habits; lack of social support.”)
- Protective Factors: What are the client’s strengths, resources, and supports that can be leveraged in treatment? This is crucial for a strengths based approach. (e.g., “Client is highly motivated for therapy; has a stable marriage; demonstrates good insight.”)
Using the 5 Ps of biopsychosocial model transforms your assessment from a simple list of facts into a dynamic, analytical tool that directly informs your diagnosis and treatment plan.
How to Write a BPS Assessment (Template and Example)
Now, let’s get to the practical application of how to write a biopsychosocial assessment. A clear structure is key. Below is a comprehensive biopsychosocial assessment template you can adapt for your own use. Following the template, you’ll find a brief example to see how it comes together in a narrative format.
Biopsychosocial Assessment Template
I. Identifying Information * Client Name: * Date of Birth: * Date of Assessment: * Therapist Name:
II. Source and Reason for Referral * Who referred the client? * What was the stated reason for the referral?
III. Presenting Problem * Describe the client’s main concerns in their own words. Include onset, duration, frequency, and severity of symptoms.
IV. History of Presenting Problem * Detailed chronological history of the issues. What were the precipitating events? How has the problem evolved over time?
V. Psychiatric and Mental Health History * Previous diagnoses, past treatment (therapy, medications), hospitalizations.
VI. Substance Use History * Current and past use of alcohol, tobacco, caffeine, illicit drugs. Include age of first use, frequency, and any history of substance abuse treatment.
VII. Medical History * Current and past medical conditions, surgeries, chronic illnesses. Note medications, diet, sleep, and exercise habits. Family medical history.
VIII. Social and Developmental History * Family of Origin: Parents, siblings, childhood environment, history of abuse/neglect. * Education: Highest level achieved, academic performance. * Employment: Current status, job history, satisfaction. * Relationships: Marital status, quality of romantic relationships, children. * Social Support: Friends, community involvement. * Cultural/Spiritual: Cultural identity, spiritual beliefs and practices. * Legal: Any past or current legal issues.
IX. Mental Status Exam (MSE) * Appearance, Behavior, Attitude, Speech, Mood, Affect, Thought Process, Thought Content, Perception, Cognition, Insight, Judgment.
X. Strengths and Protective Factors * Client’s personal strengths, coping skills, supportive relationships, resources.
XI. Clinical Summary and Case Formulation (Using the 5 Ps) * A brief, integrated summary that synthesizes the biological, psychological, and social factors. Use the 5 Ps framework here to structure your analysis.
XII. Diagnostic Impressions (DSM 5 / ICD 10) * List any diagnoses based on the information gathered.
XIII. Treatment Plan Recommendations * Initial goals for therapy, proposed modality (e.g., CBT, psychodynamic), frequency of sessions, and any referrals needed (e.g., for psychiatric evaluation, medical check up).
Biopsychosocial Assessment Example (Brief Narrative)
Client: Jane Doe, 34 year old female.
Presenting Problem: Jane presents for therapy reporting overwhelming anxiety and frequent panic attacks over the past three months, characterized by heart palpitations, shortness of breath, and a fear of “losing control.” She states, “I feel like I’m constantly on edge and can’t relax.”
Summary & Formulation: * Presenting: Generalized anxiety with panic attacks. * Precipitating: Jane was passed over for a major promotion at work three months ago, which she reports felt like a “huge failure.” * Predisposing: Jane has a family history of anxiety (mother and older sister). She describes herself as a “perfectionist” and “high achiever” since childhood, linking her self worth to her professional success. She also has a history of hypothyroidism, which was diagnosed five years ago but has been medically stable. * Perpetuating: Jane’s anxiety is maintained by her long work hours (60+ per week), excessive caffeine intake (4-5 cups of coffee daily), poor sleep (4-5 hours per night), and social withdrawal from friends. She tends to ruminate on work related fears and avoids situations where she might be evaluated. * Protective: Jane is highly insightful and motivated for treatment. She has a strong, supportive relationship with her husband and has successfully used therapy in the past to manage stress during college. She also enjoys running, which she identifies as a positive coping skill she has recently neglected.
This brief biopsychosocial assessment example shows how the information flows into a coherent narrative that points directly toward potential treatment goals, such as developing healthier coping skills, improving sleep hygiene, challenging perfectionistic thought patterns, and reengaging with her social and personal supports.
Common Mistakes to Avoid in Your BPS Assessment
Crafting a high quality BPS assessment is a skill that improves with practice. Here are a few common pitfalls to watch out for:
- The “Problem Only” Focus: It’s easy to get hyper focused on symptoms and deficits. Remember to actively inquire about and document the client’s strengths, resilience, and protective factors. Therapy is about building on what’s strong, not just fixing what’s “wrong.”
- Neglecting a Pillar: Sometimes, a client’s psychological distress is so prominent that we forget to ask detailed questions about their physical health or social environment. A client’s persistent low mood could be linked to an undiagnosed medical condition or profound social isolation. Always give equal weight to the bio, the psycho, and the social.
- Using Clinical Jargon: Write your assessment in clear, objective, and behavioral language. Avoid overly technical terms or acronyms that someone outside your specific modality might not understand. The report should be easily understood by other professionals (with client consent) who may be part of the care team.
- Being Overly Subjective: Stick to the facts. Report what the client says, what you observe, and what collateral information confirms. Differentiate clearly between objective data (e.g., “Client reports sleeping 4 hours per night”) and your clinical interpretation (e.g., “This sleep deprivation is likely exacerbating his anxiety symptoms.”).
conclusion
The biopsychosocial assessment is far more than an administrative hurdle or a piece of paperwork to check off a list. It is a dynamic and collaborative process that honors the complexity of the human experience. It is your first and best tool for building a strong therapeutic alliance, developing an accurate diagnosis, and creating a truly personalized and effective treatment plan.
By investing the time and effort to understand the intricate web of biological psychological social factors that shape a client’s life, you are laying the foundation for meaningful and lasting change. A well crafted BPS assessment is not the end of the intake process it’s the beginning of a successful therapeutic journey.