Clinical Notes AI: Reducing Burnout in Healthcare
Question on this topic? Get an instant answer from August.
Clinical Notes AI: Reducing Burnout in Healthcare
The Problem: Why Manual Documentation is Draining Healthcare
The burden of clinical documentation is more than just an annoyance; it’s a systemic issue with severe consequences. For decades, clinicians have been forced to choose between engaging deeply with their patients and meticulously documenting every detail for compliance and billing.
The statistics paint a grim picture: * Physicians spend, on average, 1.84 hours per day on EHR tasks outside of their normal work hours—the dreaded “pajama time.” source * An overwhelming 82% of clinicians point to administrative tasks, including documentation, as the leading cause of burnout. source
This isn’t just about being overworked. This constant administrative drain directly impacts the quality of patient care. When a clinician is mentally juggling note taking, they can’t be fully present. Nuances are missed. The therapeutic alliance can be strained by the persistent tapping of a keyboard. Furthermore, this intense pressure is a key reason we need solutions to reduce clinician burnout and improve the well being of our most vital healthcare professionals. The goal should be to save time on documentation so you can focus on what truly matters: your patients.
What is Clinical Notes AI and How Does it Work?
At its core, clinical notes AI is a sophisticated assistant that automates the most tedious parts of your documentation workflow. It uses a combination of advanced technologies to turn a natural conversation or dictation into a structured, compliant clinical note.
Let’s break down the magic behind it:
- Voice to Text for Clinicians: The process starts with state of the art speech recognition that accurately transcribes your spoken words.
- Ambient AI: Many advanced tools use “ambient” listening. This means the AI can capture the natural flow of a patient session (always with explicit consent) without you needing to issue commands or dictate specific sections.
- Natural Language Processing (NLP): This is the “brain” of the operation. NLP algorithms understand clinical language, context, and structure. They can identify the subjective and objective parts of a conversation and organize them into the correct format.
The result is a remarkably simple and efficient three step workflow that transforms your entire documentation process:
- Record/Capture: You record the patient session with their consent using a secure mobile app, a browser extension, or your phone. Alternatively, you can dictate a summary of your thoughts immediately after the session.
- Generate/Transcribe: The AI gets to work. Within minutes, it transcribes the entire audio and uses its intelligence to draft a complete clinical note. It can structure the information into standard formats like SOAP, DAP, or any custom template your practice uses, creating near instant automated progress notes.
- Review & Integrate: You receive a notification that your draft is ready. You quickly review the AI generated note, make any necessary edits or additions to ensure accuracy, and with a single click, transfer the final note into your EHR.
This process eliminates the need for manual typing, freeing you from the screen and allowing you to focus completely on the person in front of you.
5 Key Benefits of Adopting AI for Clinical Documentation
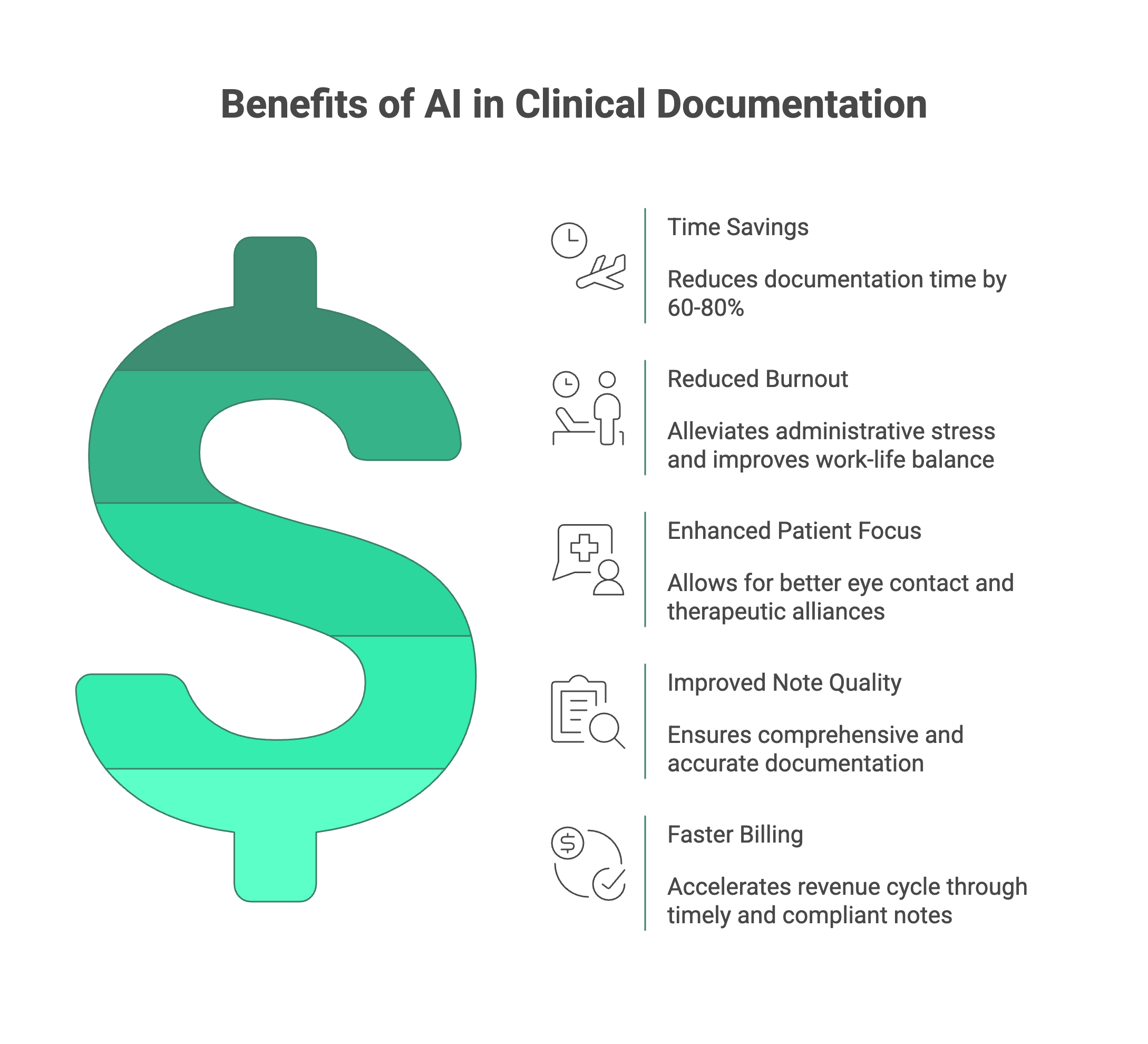
Integrating an AI medical scribe into your practice isn’t just about a minor efficiency boost. It’s a fundamental change that delivers compounding benefits for you, your practice, and your patients.
1. Massive Time Savings
This is the most immediate and tangible benefit. Clinicians using these tools consistently report saving 60-80% of the time they previously spent on notes. Imagine what you could do with an extra two or more hours back in your day. That’s more time for patients, more time for professional development, or simply more time for your own life. You will absolutely save time on documentation.
2. Reduced Burnout & Improved Well being
By slashing after hours “pajama time,” you can finally create a healthier work life balance. The mental load of constantly having a backlog of notes disappears. This directly tackles the root cause of administrative stress and is a powerful tool to reduce clinician burnout, helping you feel more energized and engaged in your work.
3. Enhanced Patient Focus and Connection
When you’re not distracted by typing, you can maintain eye contact, pick up on subtle non verbal cues, and build a stronger therapeutic alliance. Patients feel heard and valued. The technology fades into the background, allowing the human connection to take center stage. This is a core benefit of using ambient AI clinical notes.
4. Improved Note Quality & Accuracy
Human memory is fallible, especially after a long day of back to back appointments. An AI medical scribe captures the conversation verbatim, ensuring that critical details, quotes, and nuances are not forgotten. This leads to more comprehensive, accurate, and defensible automated progress notes, which is invaluable for continuity of care and compliance.
5. Faster Billing & Reimbursement
High quality, detailed, and compliant notes are the bedrock of a smooth revenue cycle. By ensuring your documentation is consistently thorough and submitted on time, you can accelerate the billing and insurance reimbursement process. This improved AI clinical documentation workflow strengthens the financial health of your entire practice.
Must Have Features: How to Choose the Right Clinical Notes AI Tool
The market for these tools is growing rapidly, and not all solutions are created equal. As you evaluate your options, there are several non negotiable features you must prioritize to ensure you choose a secure, effective, and scalable tool.
Security & Compliance: The Top Priority
In healthcare, security isn’t just a feature; it’s a foundational requirement. Any tool you consider must be built on a bedrock of security and privacy. * HIPAA Compliance: This is the absolute minimum. Look for a vendor that will sign a Business Associate Agreement (BAA). A HIPAA compliant AI scribe is not optional. * Certifications: Go beyond basic compliance. Certifications like SOC 2 and GDPR demonstrate a vendor’s commitment to rigorous, independently audited security practices. * Data Handling: Ask about their data policies. Do they offer zero data retention options? Is all data encrypted both in transit and at rest? You need a partner who treats patient data with the utmost seriousness.
Seamless EHR Integration
A tool that creates more work is no tool at all. The entire point is to streamline your process, which means the AI must work effortlessly with your existing Electronic Health Record (EHR) system. * Direct & Copy Paste: Look for solutions that offer robust EHR integration AI. The best tools provide one click integrations with popular systems like Simple Practice, Cliniko, AthenaHealth, Cerner, and more. At a minimum, they should offer a seamless and formatted copy paste function that works with any web based EHR.
Customization and Template Flexibility
Your notes are unique to your specialty, your style, and your practice’s requirements. A one size fits all approach doesn’t work. * Custom Templates: The right tool will allow you to create and save your own templates. Whether you use SOAP, DAP, GIRP, or a completely custom format, the AI should be able to structure the output to match your exact needs. This is particularly crucial for AI for behavioral health notes, where specific formats are often required.
Specialty Specific Training
General dictation software often stumbles over the specific terminology and nuances of healthcare, especially in mental and behavioral health. * Purpose Built for Healthcare: Seek out tools that have been specifically trained on clinical language. The best solutions are often those designed for niches. For example, an AI note taking for therapists will be far more effective at understanding and documenting a therapy session than a generic transcription service. This specialized training is key for accuracy.
Accessibility and Ease of Use
The tool should fit into your workflow, not the other way around. * Multi Platform Access: Check for flexibility. Does it offer a browser extension that works directly in your EHR? Is there a dedicated mobile app for iOS and Android so you can capture notes on the go? The more accessible the tool, the more likely you are to use it consistently. The use of a dedicated app is a huge plus for any HIPAA compliant AI scribe.
Your Partner in Care, Not Your Replacement
The rise of AI clinical documentation is one of the most exciting advancements in healthcare technology, offering a real solution to the burnout epidemic. By handling the administrative drudgery, these tools empower you to reclaim your time and focus on the work you were trained to do: providing exceptional care.
It’s crucial to remember that your clinical judgment remains central. This technology is an incredibly powerful assistant, a partner that ensures nothing gets missed, but you are always in the driver’s seat. You review, you edit, and you sign off.
If you’re ready to end the cycle of “pajama time” and rediscover the joy in your practice, the next step is to see this technology in action for yourself.
Ready to transform your workflow? Start a free trial or book a demo today to experience the power of AI driven clinical notes firsthand.