The Best Medical Transcription Software of 2026
Question on this topic? Get an instant answer from August.
The Best Medical Transcription Software of 2026
What is Medical Transcription Software?
Let’s clear up a common point of confusion. When you hear “transcription,” you might picture old school medical dictation software, where a doctor records their voice into a device, and someone else (or a basic program) types it up later.
Modern medical transcription software is a different beast entirely. It uses a sophisticated blend of technologies:
- Artificial Intelligence (AI): The brain that understands context and structure.
- Automatic Speech Recognition (ASR): The ears that accurately capture spoken words.
- Natural Language Processing (NLP): The interpreter that deciphers medical meaning, identifies speakers, and extracts key clinical data.
Think of it this way: traditional medical dictation software is like a tape recorder. Modern transcription software is like having a super intelligent, invisible scribe in the room with you. This AI medical scribe doesn’t just turn voice into a wall of text. It understands the nuances of a clinical conversation, differentiates between the clinician and the patient, and can even structure the output into a perfect SOAP note.
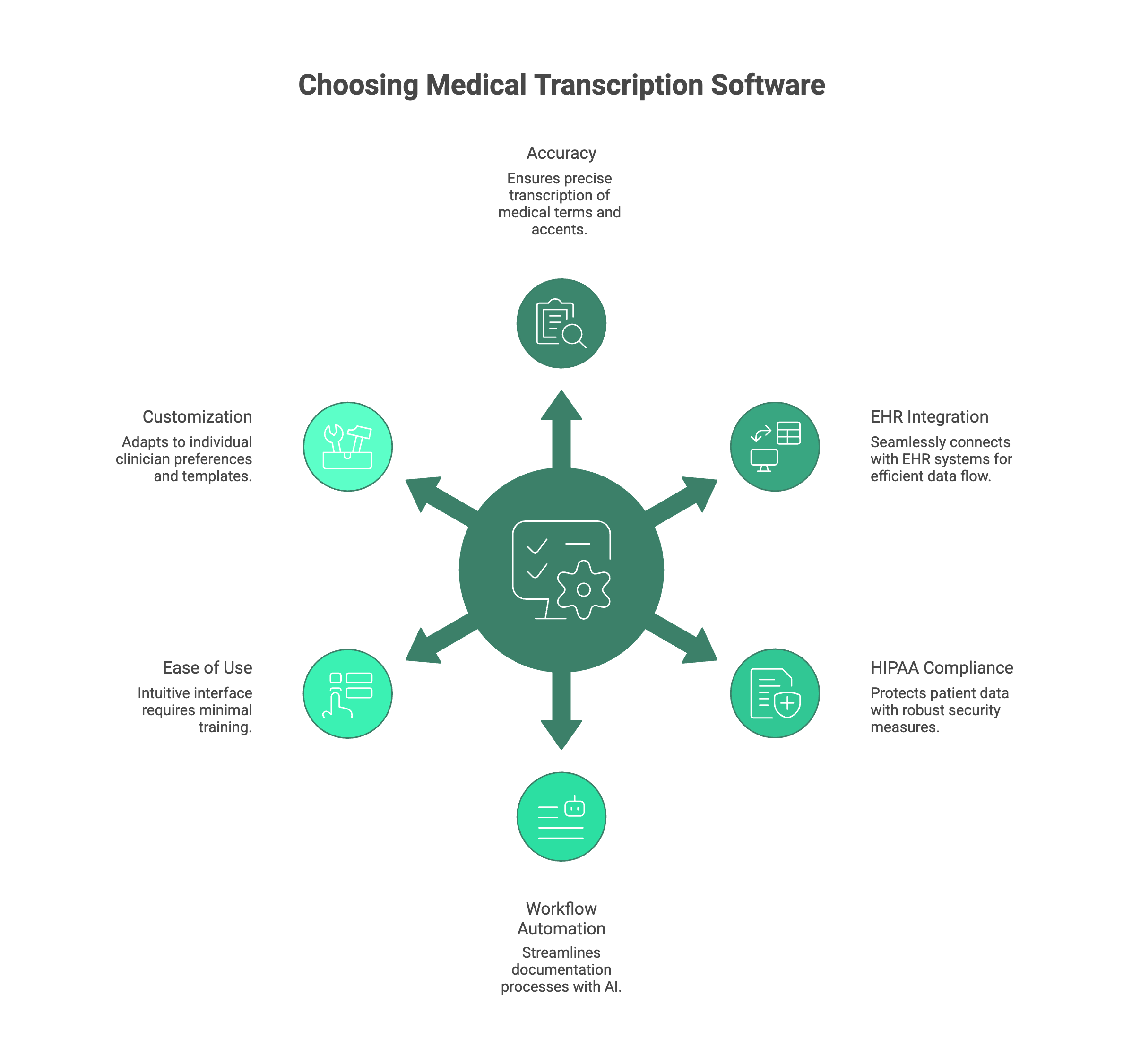
Key Features to Look for When Choosing Medical Transcription Software
With a growing number of options, it’s crucial to know what separates a good tool from a great one. Here are the non negotiable features you should evaluate.
Accuracy & Medical Vocabulary
The software’s primary job is to be accurate. It must have an extensive, specialty specific vocabulary to correctly identify complex drug names, procedures, and diagnoses. The best systems can handle various accents, speaking speeds, and even background noise while maintaining over 98% accuracy.
EHR/EMR Integration
This is paramount. A tool that can’t communicate with your Electronic Health Record (EHR) system simply moves the bottleneck. Look for seamless, one click EHR integration medical transcription. The software should be able to push structured notes directly into the correct fields in systems like Epic, Cerner, athenahealth, eClinicalWorks, and others without tedious copy pasting.
HIPAA Compliance & Security
Patient data is sacred. There is zero room for compromise here. The software you choose must offer HIPAA compliant transcription. This means providing enterprise grade data encryption (both in transit and at rest), clear Business Associate Agreements (BAAs), and robust data privacy policies. Ensure the provider has a strong security posture.
Workflow Automation
The most powerful tools go beyond simple transcription. They automate entire documentation workflows. Can the software generate automated SOAP notes from a natural conversation? Can it suggest relevant ICD 10 and CPT codes based on the encounter? Can it draft referral letters or patient instructions? This is where you see the most significant time savings. The evolution of AI for clinical documentation has made this a reality.
Ease of Use & Accessibility
A tool designed to save you time shouldn’t require weeks of training. The best platforms are intuitive, with a clean user interface. Look for solutions that are easy to set up (many modern cloud based tools require no IT support) and accessible on multiple devices, like a desktop computer or a mobile app for your phone or tablet.
Customization & Adaptability
Every clinician has a unique style of speaking and documenting. The software should be able to learn your preferences, acronyms, and templates over time. Great physician dictation software adapts to you, not the other way around. Look for the ability to create custom templates and macros to fit your specific workflow.
The Best Medical Transcription Software of 2026
We’ve evaluated the top players in the market based on the criteria above. Here are the best solutions for reducing your documentation burden today.
1. DeepScribe
- Best for: Ambient, real time AI medical scribing.
- What it does: DeepScribe is a leader in the ambient AI space. You simply talk with your patient naturally, and DeepScribe listens in the background (via a smartphone or device in the room), generating a complete, accurate medical note in real time. It’s designed to be a completely hands free experience.
- Who it’s for: Primary care providers, specialists, and any clinician in a busy practice who wants to completely eliminate manual note taking during patient visits.
- Pros:
- Fully ambient and hands free, allowing for better patient focus.
- High accuracy and adapts to your personal documentation style over time.
- Offers robust EHR integration medical transcription with leading platforms.
- Provides real time medical transcription so notes are ready immediately post visit.
- Cons:
- Requires a quiet, controlled environment for optimal accuracy.
- Pricing is not publicly listed and requires a custom quote.
- Pricing: Available upon request; requires a demo.
2. Dragon Medical One
- Best for: Enterprise grade cloud based medical dictation.
- What it does: From Nuance (now a part of Microsoft), Dragon Medical One is one of the most established names in physician dictation software. It’s a cloud based solution that allows clinicians to dictate notes, emails, and other documents directly into any application on their computer with high accuracy.
- Who it’s for: Large hospitals and health systems that need a reliable, scalable, and secure dictation tool that integrates deeply into enterprise environments.
- Pros:
- Exceptional accuracy for medical terminology across over 90 specialties.
- Consistent and user friendly interface.
- Lightweight cloud based platform that works across various devices.
- Strong reputation and widely used in major health systems.
- Cons:
- Primarily a dictation tool, not an ambient scribe; it doesn’t automatically structure notes from a conversation.
- Can be more expensive than other solutions, especially for smaller practices.
- Pricing: Typically sold through resellers; requires a custom quote.
3. Freed AI Scribe
- Best for: Simple and effective automated clinical documentation for private practices.
- What it does: Freed AI Scribe focuses on doing one thing exceptionally well: listening to your patient visits and generating clear, concise, and accurate SOAP notes. It’s designed to be incredibly easy to use, with a simple workflow: record, review, and export to your EHR.
- Who it’s for: Clinicians in smaller private practices (especially in mental health, primary care, and pediatrics) who need a straightforward, reliable, and affordable AI medical scribe.
- Pros:
- Very easy to set up and use with minimal learning curve.
- Generates well structured and easy to read summaries and notes.
- HIPAA compliant and built with security as a top priority.
- Transparent and affordable pricing.
- Cons:
- Fewer bells and whistles compared to all in one platforms like Lindy.
- Direct EHR integrations are still growing.
- Pricing: Starts at $99/month.
4. Sunoh.ai
- Best for: Deep integration with the eClinicalWorks EHR.
- What it does: Developed by the creators of eClinicalWorks (ECW), Sunoh.ai is an AI powered ambient listening technology designed to work seamlessly within the ECW ecosystem. It listens to the patient conversation and transcribes it in real time, populating the relevant sections of the EHR note.
- Who it’s for: Medical practices that are already using or plan to use the eClinicalWorks EHR.
- Pros:
- Unparalleled, native integration with the ECW platform.
- Enhances the workflow for existing ECW users.
- Captures both audio and video for comprehensive documentation.
- Cons:
- Its primary value is tied to the eClinicalWorks EHR; not a standalone solution for practices on other systems.
- Less flexible than platform agnostic tools.
- Pricing: Available through eClinicalWorks.
5. Heidi Health
- Best for: AI powered clinical workflow support for Australian GPs.
- What it does: Heidi Health is an AI powered platform that acts as a clinical co pilot. It includes a medical scribe feature that creates notes from conversations but also helps with differential diagnoses, patient education, and administrative tasks. It’s tailored specifically to the Australian healthcare system.
- Who it’s for: General Practitioners and specialists in Australia looking for an AI tool that understands their unique clinical and administrative workflows.
- Pros:
- Designed specifically for the Australian healthcare context.
- Offers features beyond transcription, including clinical decision support.
- Provides high quality real time medical transcription.
- Cons:
- Focused on the Australian market, so it may not be suitable for clinicians elsewhere.
- Still an emerging platform compared to more established global players.
- Pricing: Offers a free tier with paid plans for more features.
6. Amazon Transcribe Medical
- Best for: Developers building custom healthcare applications.
- What it does: Amazon Transcribe Medical is not an out of the box software for clinicians. It’s a powerful medical speech to text API from Amazon Web Services (AWS) that developers can use to build their own healthcare applications. It provides highly accurate, real time transcription of medical speech.
- Who it’s for: Healthcare organizations, startups, and IT teams with the development resources to build a custom solution on top of AWS’s powerful transcription engine.
- Pros:
- Industry leading accuracy for medical speech.
- Scalable and reliable, backed by the power of AWS.
- Fully managed service, reducing infrastructure overhead for developers.
- Cons:
- It is not a ready to use application for doctors; it’s a developer tool.
- Requires significant technical expertise to implement.
- Pricing: Pay as you go based on the amount of audio transcribed.
Frequently Asked Questions
1. What’s the difference between medical dictation and transcription software?
The main difference is intelligence and automation. Traditional medical dictation software simply converts spoken words into text. Modern medical transcription software, powered by AI for clinical documentation, understands context, separates speakers, and automatically structures the text into a clinically useful format like a SOAP note.
2. Is medical speech recognition software HIPAA compliant?
Yes, all reputable solutions designed for clinical use are. Vendors should be willing to sign a Business Associate Agreement (BAA) and provide clear documentation on their security measures. Always verify a platform’s commitment to HIPAA compliant transcription before using it.
3. Do I need special equipment to use this software?
No. Most modern platforms are cloud based and work with the existing hardware you already have. You can typically use the microphone on your computer, smartphone, or a simple external USB microphone. No complex installation or IT support is required.
4. How accurate is medical speech to text software?
Accuracy has improved dramatically in recent years. The leading tools on this list consistently achieve accuracy rates of 98-99% or higher, often outperforming human transcriptionists, especially with clear audio and a good microphone. They are specifically trained on vast medical vocabularies to ensure precision.
5. Can I connect dictation software to my EHR system?
Absolutely. This is a critical feature. The best solutions offer deep integrations with major EHRs like Epic and Cerner, allowing you to push completed notes directly into the patient’s chart with a single click, saving significant time and eliminating manual data entry.
Conclusion
The days of spending hours on after hours charting are numbered. The administrative burden that has plagued medicine for decades is finally being lifted by intelligent, intuitive technology. By adopting the right medical transcription software, you can slash your documentation time, reduce errors, improve the quality of your notes, and most importantly reconnect with the passion that brought you to medicine in the first place.